Squamous cell carcinoma (SCC) is a cancer of a kind of epithelial cell, the squamous cell. These cells are the main part of the epidermis of the skin, and this cancer is one of the major forms of skin cancer. However, squamous cells also occur in the lining of the digestive tract, lungs, and other areas of the body, and SCC occurs as a form of cancer in diverse tissues, including the lips, mouth, esophagus, urinary bladder, prostate, lung, vagina, and cervix, among others.
Squamous cell carcinoma is the second-most common cancer of the skin (after basal cell carcinomaBasal Cell Carcinoma but more common than melanoma). It usually occurs in areas exposed to the sun. Sunlight exposure and immunosuppression are risk factors for SCC of the skin, with chronic sun exposure being the strongest environmental risk factor. The risk of metastasis is low, but is much higher than with basal cell carcinoma. Squamous cell cancers of the lip and ears have high rates of local recurrence and distant metastasis (20–50%).
Squamous cell cancers of the skin in individuals on immunotherapy or suffering from lymphoproliferative disorders (i.e. leukemia) tend to be much more aggressive, regardless of their location.
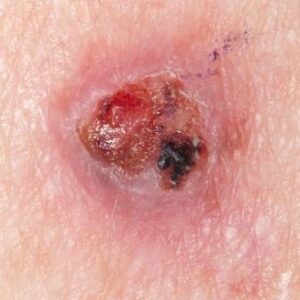
SCCs represent about 20% of the non-melanoma skin cancers, but due to their more obvious nature and growth rates, they represent 90% of all head and neck cancers that are initially presented. The vast majority of SCCs are those of the skin, and like all skin cancers, are the result of ultraviolet exposure. SCCs usually occur on portions of the body commonly exposed to the Sun; the face, ears, neck, hands, or arm. The main symptom is a growing bump that may have a rough, scaly surface and flat reddish patches. Unlike basal cell carcinomas, SCCs carry a significant risk of metastasis, often spreading to the lymph nodes, and are thus more dangerous. During its earliest stages, it is sometimes known as Bowen’s disease.

Symptoms are highly variable depending on the involved organs. SCC of the skin begins as a small nodule and as it enlarges the center becomes necrotic and sloughs and the nodule turns into an ulcer.
– The lesion caused by SCC is often asymptomatic
– Ulcer or reddish skin plaque that is slow growing
– Intermittent bleeding from the tumor, especially on the lip
– The clinical appearance is highly variable
– Usually the tumor presents as an ulcerated lesion with hard, raised edges
– The tumor may be in the form of a hard plaque or a papule, often with an opalescent quality, with tiny blood vessels
– The tumor can lie below the level of the surrounding skin, and eventually ulcerates and invades the underlying tissue
– The tumor commonly presents on sun-exposed areas (e.g. back of the hand, scalp, lip, and superior surface of pinna)
– On the lip, the tumor forms a small ulcer, which fails to heal and bleeds intermittently
– Evidence of chronic skin photodamage, such as multiple actinic keratoses (solar keratoses)
– The tumor grows relatively slowly
– Unlike basal cell carcinoma (BCC), squamous cell carcinoma (SCC) has a substantial risk of metastasis
– Risk of metastasis is higher in SCC arising in scars, on the lower lips or mucosa, and occurring in immunosuppressed patients.
About one-third of lingual and mucosal tumors metastasize before diagnosis (these are often related to tobacco and alcohol use)
Visual diagnosis of squamous cell carecinoma is still the most common method employed by health professionals.
Mr Stanley Loo is a specialist in the management of squamous cell carcinoma’s. He will fully asses the lesion and all other areas of potential spread at the initial consultation.
Treatment of squamous cell carcinoma’s are primarily surgery however other treatments may be beneficial in certain cases (Mr Loo will explain this to you in the consultation at Auckland Plastic Surgery Group, Unit 6 / 31 Highbrook Drive, Highbrook, Auckland 2013 Ph (09) 220 2580 and perform the surgery at either Auckland Plastic Surgery Group, Kakariki Hospital or Ormiston Hospital). Diagnosis is confirmed with a biopsy (small surgical procedure). If the diagnosis of squamous cell carcinoma is confirmed further investigations may be required.
Non-surgical options for the treatment of cutaneous SCC include topical chemotherapy, topical immune response modifiers, photodynamic therapy (PDT), radiotherapy, and systemic chemotherapy. The use of topical therapy, such as immune response modifiers and PDT is generally limited to premalignant (i.e., AKs) and in situ lesions. Radiation therapy is a primary treatment option for patients in whom surgery is not feasible and is an adjuvant therapy for those with metastatic or high-risk cutaneous SCC.
In cases where there is spread to other areas, Mr Stanley Loo will discuss the treatment plan in the consultation.
Regular follow up is very important in the long term management of squamous cell carcinoma and should be done by an appropriate health professional. Mr Loo will follow you up at his rooms (Auckland Plastic Surgery Group) and arrange all appropriate investigation as required.
If you would like to discuss this further a consultation can be made with Mr Stanley Loo at Auckland Plastic Surgery Group, Unit 6 / 31 Highbrook Drive, Highbrook, Auckland 2013 Ph (09) 220 2580